There are other ways to narrow down the location of the problem as well:
- The muscles will be painful to palpation at a specific vertebral segment and may even refer pain down the leg when palpated with deeper pressure.
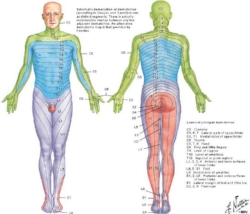
- Reflexes may be diminished. A slow or non-existent patellar tendon reflex corresponds with lumbar spinal nerve L4.
- Muscles may test weaker on the affected side which may indicate an injury to a particular spinal level or nerve. An example of this would be weakness in the calf muscles (can’t lift up on to the toes) which are controlled by the first two sacral nerves (S1 and S2 on the chart).
So below are a couple great examples of a number of these factors all lining up and how quickly the pain and loss of function can be addressed.
Case Study #1
The patient in this case had left sided low back pain and pain running down through the back of her hip and leg to the mid-calf. She felt a ‘pop’ in her back and immediate leg pain as a result of pushing and twisting trying to put a heavy object in the back of her truck. She is an avid runner but even standing and walking significantly increase her pain after 10 minutes.
Exam
So here is what I found:
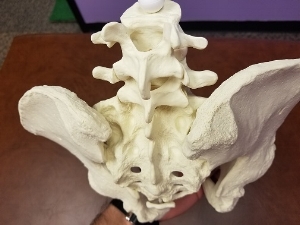
- Symptoms following the S1 and 2 dermatomes down the back of the left leg
- Increased muscle tone/spasm at the S1 and S2 levels of the spine, and these muscles are tender to palpation.
- ‘Springing’ or pushing down on the S1/S2 vertebrae reproduced the symptoms into the back of her hip/upper thigh.
- She could do only 12 calf raises on her left leg while doing 25 on the right side (this muscle corresponds with S1 and S2 nerves).
- Achilles reflexes normal (S1 reflex)
It’s nice when everything points back to a specific level or two like that. Doesn’t always work that way but when it does it makes me much more confident that we can knock this out quickly.
Treatment
In this case I chose to use dry needling to address the muscles at the S1 and S2 spinal levels on both sides of the spine. Once the needles were placed I attached an electrical stimulation unit and she just relaxed for 10 minutes. Dry needling in conjunction with e-stim are shown in the research to decrease tone within the muscles as well as alleviate pain through a number of local and global factors.
The patient was instructed in two exercises that had multiple purposes:
- decrease pain through relaxation of the over worked muscles of the back and anterior hip
- facilitate improved stability through the lumbar spine and pelvis
Results
The patient had near full resolution of symptoms for two days after the first session. Her exercises relieved her pain at home and she could walk as much as she wanted. She tried to run on the third day but was unable due to pain.
We repeated the same dry needling + e-stim treatment during the second visit and followed it up by progressing her exercise program.
The patient cancelled her appointment the next week as she reported being completely pain free and back to running.
Case Study #2
The patient in this case presented to our clinic with pain shooting into the front of his hip and groin as well as down the front and side of his thigh. He also reported minor back pain but it was nothing compared to the pain in his leg. The patient reported having this pain on and off over the past couple years especially when exercising but recently it was much more constant and severe. In the past he had been diagnosed with IT Band syndrome (pain laterally in the hip and thigh might make you think that), and more recently with a hip flexor strain (could also make sense now that he was having more pain into the front of the hip and groin).
Exam
- Minimal tenderness to the ‘hip flexor’ muscles anteriorly, slight weakness with manual muscle testing but no pain (probably not a hip flexor strain).
- Moderate tenderness and active trigger points in the lateral hip musculature that referred pain down the lateral thigh to the knee (could be part of IT Band syndrome).
- Springing of the lumbar vertebrae at L2 and L3 reproduced the typical symptoms he felt into his anterior hip/groin as well as lateral thigh (Bingo!)
Treatment
Dry needling was performed at the levels of L2 and L3 along with electric stimulation for 10 minutes, and followed up with IASTM to decrease tone and improve mobility of the superficial fascia and muscles of the mid and lower back.
A couple exercises were given to maintain, and hopefully even improve, the mobility gained through the spine and hips as a result of the dry needling and IASTM.
Results
The patient reported a significant decrease in the anterior hip and groin symptoms as well as a moderate improvement in lateral hip and thigh symptoms.
During the second treatment session I decided to treat the muscles of the lateral hip as well since they also referred pain into the lateral thigh. This was done with by dry needling + e-stim just like we had done in the low back.
By the third treatment session a few days later the patient was reporting a significant reduction in lateral hip and thigh symptoms as well.
Final Thoughts
It took a few more treatments to completely resolve this patient’s symptoms but it’s nice to see an immediate decrease in symptoms to know that you are treating the right areas. With a thorough evaluation process it wasn’t hard to figure out that the patient’s symptoms were primarily coming from his spine which was quite a different diagnosis than what was previously thought.
If this sounds similar to you or would like some assistance in your recovery, then click the link below to receive a FREE discovery session.