Injuries can be frustrating, but they happen to everyone.
It’s very common to think when you have an injury, that you are alone. But that couldn’t be further from the truth as many people suffer from injuries and lingering pain.
So your understanding of how injuries occur is the best defense you can have against getting injured in the first place. Furthermore, this knowledge will also be very helpful to get out of pain!
I made the video below, because this is often a question I get asked by patients. Furthermore, I happen to run a continuing education company for rehab professionals and strength coaches (Sports Rehab Expert) and this concept is something that I spend a lot of time trying to drive into people’s minds so that it becomes common knowledge.
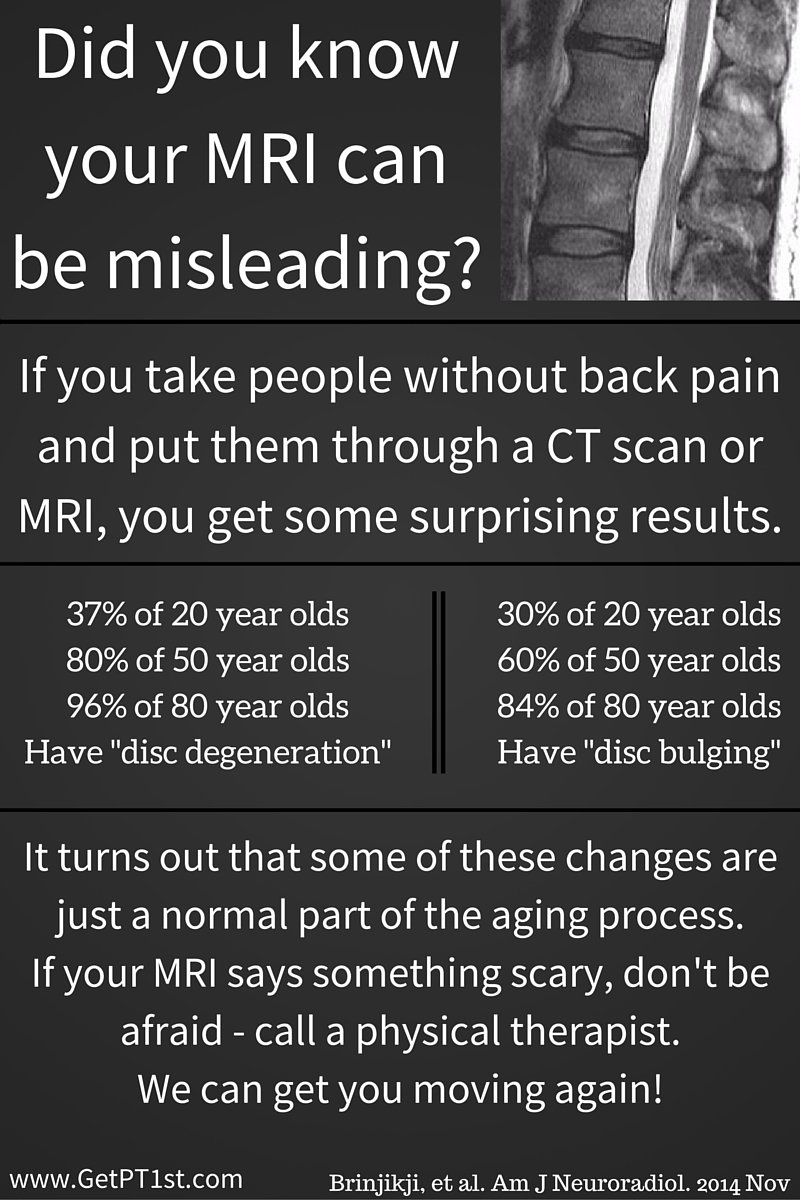
As you will see, the concept is not that unique or novel. It’s actually pretty common sense when you look at it this way. But unfortunately the medical community likes to over complicate problems and make the process seem more complicated then it really is…..
Aside from how an injury happens, the second most common question I get asked is “how I can help?”
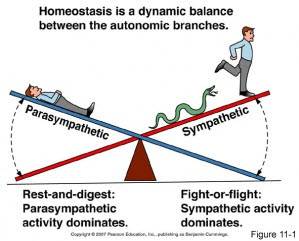
When you look at the equation of Stress vs. Capacity, here is what we can help you do!
Building Capacity = Help you rebuild the tissues compromised in the fastest most efficient way through very specific/direct exercises. This depends on your current capacity and as that improves, the activity should become more challenging along the way. So we help guide you to make better decisions on WHEN, HOW MUCH, and WHAT to do. It’s also important to take into consideration the activities you would like to return back to doing. The more specific we can get these exercises to mimic what you would like to do, the better shot you have to return back to them!
Tissue Stress = First this involves modifying or sometimes removing provocative factors. Secondary to this is show you through exercise how to more efficiently distribute stress across your entire body instead of in one particular area. This is where range of motion and coordination come into play.
Recovery = We also perform hands on treatments such as massage, mobilization, cupping, dry needling to help the recovery process and start removing tissue stress quicker so that the capacity bucket doesn’t start to overflow and help you to continue and be more active (which ultimately starts help building the capacity up when combined with previous mentioned interventions).
I hope you have found this to help provide clarity on what the problem might be and what you can start doing about it. Also, feel free to share this if you feel it could help a friend!
If you would like more information on how we can help, I would encourage you to set up a FREE Discovery session to meet :)